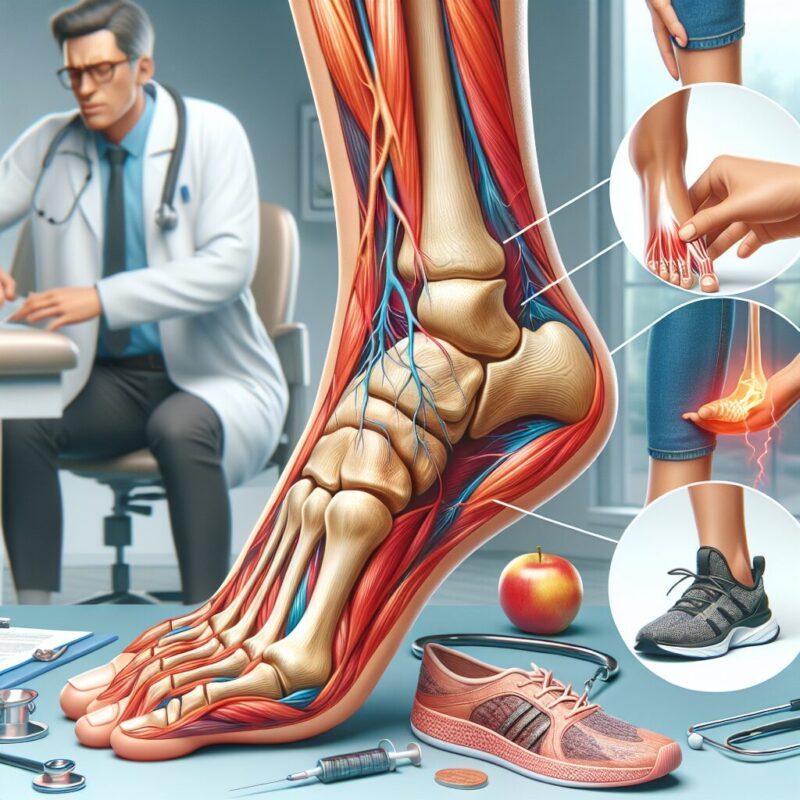
Plantar fasciitis is a common foot condition that causes heel pain and discomfort. It occurs when the ligament that connects the heel bone to the toes becomes inflamed or strained. This condition can be quite debilitating, making it difficult to walk or engage in physical activities. However, knowing when to see a podiatrist for plantar fasciitis is crucial in managing the condition effectively.
One unique fact about plantar fasciitis is that it predominantly affects runners and athletes who engage in high-impact activities. The repetitive stress placed on the plantar fascia during these activities can lead to its inflammation and subsequent heel pain. Additionally, individuals who are overweight or have abnormal foot mechanics, such as flat feet or high arches, are also at a higher risk of developing this condition.
When it comes to seeking medical help for plantar fasciitis, timing is essential. If left untreated, the condition can worsen and become chronic, leading to long-term pain and disability. Therefore, it is crucial to recognize the early signs and symptoms and consult with a podiatrist promptly. In the following section, we will discuss the key takeaways regarding when to see a podiatrist for plantar fasciitis and the available treatment options to alleviate the pain and promote healing.
What you should know
1. Plantar fasciitis is a common condition that causes pain in the heel and bottom of the foot due to inflammation and irritation of the plantar fascia.
2. Seeking medical attention from a podiatrist is recommended if symptoms persist for more than a few weeks or if the pain is severe and affects daily activities.
3. Podiatrists can accurately diagnose plantar fasciitis through a physical examination, reviewing medical history, and possibly ordering imaging tests.
4. Treatment options for plantar fasciitis may include rest, physical therapy exercises, orthotics, night splints, and in some cases, corticosteroid injections or surgery.
5. Early intervention and proper treatment by a podiatrist can help relieve pain, reduce inflammation, and prevent further complications associated with plantar fasciitis.
When should I see a podiatrist for plantar fasciitis?
The best time to see a podiatrist for plantar fasciitis is when you experience persistent heel pain that does not improve with rest or self-care measures. Plantar fasciitis is a common condition characterized by inflammation of the plantar fascia, a thick band of tissue that connects the heel bone to the toes. It typically causes stabbing pain in the heel, especially in the morning or after prolonged periods of rest. While mild cases can often be managed at home, it is important to seek professional help if the pain persists or worsens.
One key indicator that you should see a podiatrist is if the pain interferes with your daily activities or limits your ability to walk or exercise. Additionally, if you have tried conservative treatments such as rest, ice, stretching exercises, and over-the-counter pain medications without relief, it is advisable to consult a podiatrist. They can provide a comprehensive evaluation, diagnose the underlying cause of your plantar fasciitis, and recommend appropriate treatment options.
Furthermore, if you notice any signs of infection, such as redness, warmth, swelling, or drainage from the affected area, it is crucial to seek immediate medical attention. These symptoms may indicate a more serious condition or a secondary infection that requires prompt treatment. Remember, early intervention and proper management can help prevent long-term complications and promote faster recovery.
Treatment options for plantar fasciitis
When it comes to treating plantar fasciitis, there are several options available depending on the severity and duration of your symptoms. The primary goal of treatment is to reduce pain, inflammation, and promote healing of the plantar fascia. Here are some common treatment approaches:
1. Conservative measures: In most cases, plantar fasciitis can be effectively managed with conservative measures. These may include rest, avoiding activities that worsen the pain, applying ice packs, wearing supportive shoes or orthotics, and performing stretching exercises to improve flexibility and strengthen the foot muscles. Over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can also provide temporary relief.
2. Physical therapy: If conservative measures do not provide sufficient relief, a podiatrist may recommend physical therapy. This can involve various techniques such as ultrasound, electrical stimulation, and exercises tailored to your specific condition. Physical therapy aims to reduce pain, improve flexibility, and strengthen the muscles surrounding the plantar fascia.
3. Extracorporeal shockwave therapy (ESWT): ESWT is a non-invasive procedure that uses shockwaves to stimulate healing in the affected area. It has shown promising results in relieving plantar fasciitis pain and promoting tissue regeneration. During the procedure, high-energy sound waves are directed to the heel, helping to break down scar tissue and stimulate blood flow.
Preventing plantar fasciitis and self-care tips
Prevention is always better than cure, and there are steps you can take to reduce the risk of developing plantar fasciitis or prevent its recurrence. Here are some self-care tips and preventive measures:
1. Wear supportive footwear: Choose shoes that provide adequate arch support, cushioning, and shock absorption. Avoid high heels and shoes with worn-out soles, as they can contribute to foot strain and increase the risk of plantar fasciitis.
2. Maintain a healthy weight: Excess weight puts additional stress on your feet and can contribute to the development or worsening of plantar fasciitis. Maintain a healthy weight through a balanced diet and regular exercise to reduce the strain on your feet.
3. Warm-up and stretch: Before engaging in physical activities or exercises, warm up your muscles and perform stretching exercises to improve flexibility and reduce the risk of injury. Focus on stretching the calf muscles and the plantar fascia itself.
4. Gradual increase in activity: If you are starting a new exercise routine or increasing the intensity of your workouts, do so gradually. Sudden changes in activity levels can strain the plantar fascia and lead to injury.
5. Listen to your body: Pay attention to any signs of foot pain or discomfort. If you experience heel pain, rest and give your feet time to recover. Ignoring the symptoms and pushing through the pain can worsen the condition.
By following these preventive measures and seeking timely medical attention when needed, you can reduce the risk of developing plantar fasciitis and ensure prompt treatment if it does occur.
1. What is plantar fasciitis?
Plantar fasciitis is a common foot condition that causes pain and inflammation in the plantar fascia, a thick band of tissue that runs along the bottom of the foot. It is often characterized by sharp pain in the heel or arch of the foot, especially when taking the first steps in the morning or after periods of rest.
2. How do I know if I have plantar fasciitis?
If you are experiencing persistent heel or foot pain, especially in the morning or after prolonged periods of standing or walking, it is possible that you have plantar fasciitis. Other common symptoms include tenderness, swelling, and aching in the affected area. However, it is important to consult with a podiatrist for an accurate diagnosis and appropriate treatment plan.
3. When should I see a podiatrist for plantar fasciitis?
If you have been experiencing foot pain for more than a few weeks, or if the pain is severe and affecting your daily activities, it is recommended to see a podiatrist. Additionally, if you have tried home remedies such as rest, ice, stretching, and over-the-counter pain medications without relief, it is advisable to seek professional medical attention.
4. What can a podiatrist do for plantar fasciitis?
A podiatrist is a foot specialist who can provide a comprehensive evaluation and diagnosis of your foot condition. They may recommend various treatment options such as custom orthotics, physical therapy, stretching exercises, night splints, or corticosteroid injections. In severe cases, surgical intervention may be considered as a last resort.
5. Can plantar fasciitis go away on its own?
In some cases, plantar fasciitis may resolve on its own with conservative treatments such as rest, ice, stretching, and wearing supportive footwear. However, it is important to note that the condition can become chronic if left untreated or if the underlying causes are not addressed. Seeking professional medical advice can help prevent long-term complications.
6. How long does it take to recover from plantar fasciitis?
The recovery time for plantar fasciitis varies depending on the individual and the severity of the condition. With proper treatment and adherence to a recommended treatment plan, many people experience significant improvement within a few months. However, it is important to continue with preventive measures and follow-up appointments to prevent recurrence.
7. Can I treat plantar fasciitis at home?
While there are several home remedies that can help alleviate the symptoms of plantar fasciitis, it is advisable to consult with a podiatrist for an accurate diagnosis and personalized treatment plan. Home treatments such as rest, ice, stretching exercises, and over-the-counter pain medications can provide temporary relief, but professional guidance can ensure effective and long-lasting results.
8. What are the risk factors for developing plantar fasciitis?
There are several risk factors that can increase the likelihood of developing plantar fasciitis. These include obesity, high-impact activities such as running or jumping, occupations that require prolonged standing or walking, flat feet or high arches, and wearing improper footwear. Understanding these risk factors can help in preventing the condition or seeking early treatment.
9. Can I continue exercising with plantar fasciitis?
It is important to modify your exercise routine if you have plantar fasciitis to avoid exacerbating the condition. High-impact activities should be avoided, and low-impact exercises such as swimming or cycling can be beneficial. Consulting with a podiatrist can help determine the appropriate modifications to your exercise routine and provide guidance on when it is safe to resume regular activities.
10. How can I prevent plantar fasciitis?
There are several preventive measures that can help reduce the risk of developing plantar fasciitis. These include maintaining a healthy weight, wearing supportive and properly-fitted footwear, avoiding high-impact activities on hard surfaces, warming up and stretching before exercise, and gradually increasing the intensity of physical activities. Additionally, regular foot care and seeking prompt medical attention for any foot pain or discomfort can help prevent the condition from worsening.